What NICE guidance means for antimicrobial wound dressings
 ;
;
We’re excited to share that the latest evaluation from the National Institute for Health and Care Excellence (NICE) provides important clarity on the use of topical antimicrobial dressings such as Aquacel® Ag+ Extra™ for infected leg ulcers.
The guidance forms part of NICE’s Late-Stage Assessment (LSA) framework, which evaluates categories of technologies already in widespread NHS use within the UK and Ireland.
Key findings:¹⁻²
- Silver agents assumed to be used up to 12 weeks
- Evidence favours silver agents for achieving complete wound healing
- The faster patients progress to healing, the more likely that outcome will be cost-effective
What does the NICE LSA say?
The LSA looked at a range of clinical evidence, including randomised controlled trials (RCTs), real-world case studies, and expert opinion. Aquacel® Ag+ Extra™, with its three-component formula, was identified as a dressing that may offer better patient outcomes and faster healing times in the presence of infection risk.
NICE's LSA highlights Aquacel® Ag+ Extra™ as a clinically effective and potentially cost-saving solution for wounds where infection or biofilm is suspected. Its evaluation recognised that certain silver dressings, particularly those designed with biofilm-disrupting technologies, such as More Than Silver™ technology can play a vital role in hard-to-heal wound care.
Why this matters for HCPs
With increasing focus on antimicrobial stewardship, many clinicians have been cautious about silver dressings, including the long-standing myth that silver-containing dressings can only be used for 2 weeks.
NICE’s latest review provides reassurance that, when used appropriately, dressings like Aquacel® Ag+ Extra™ offer measurable benefits and are assumed for use for 12 weeks, reviewing every 2 weeks and to keep using if needed.³
The biofilm battle
Biofilms are mixed communities of bacteria and other microorganisms living together⁴ and when free floating bacteria attach to a surface, this is when they can begin forming a biofilm. Biofilm is a major barrier to wound healing, thought to be present in almost 8 out of 10 hard-to-heal wounds⁵ – therefore it should be assumed present in every hard-to-heal wound.⁶
Biofilm is not always visible to the naked eye⁷ and can be difficult to remove, even after aggressive debridement, even reforming within 24 hours.⁸
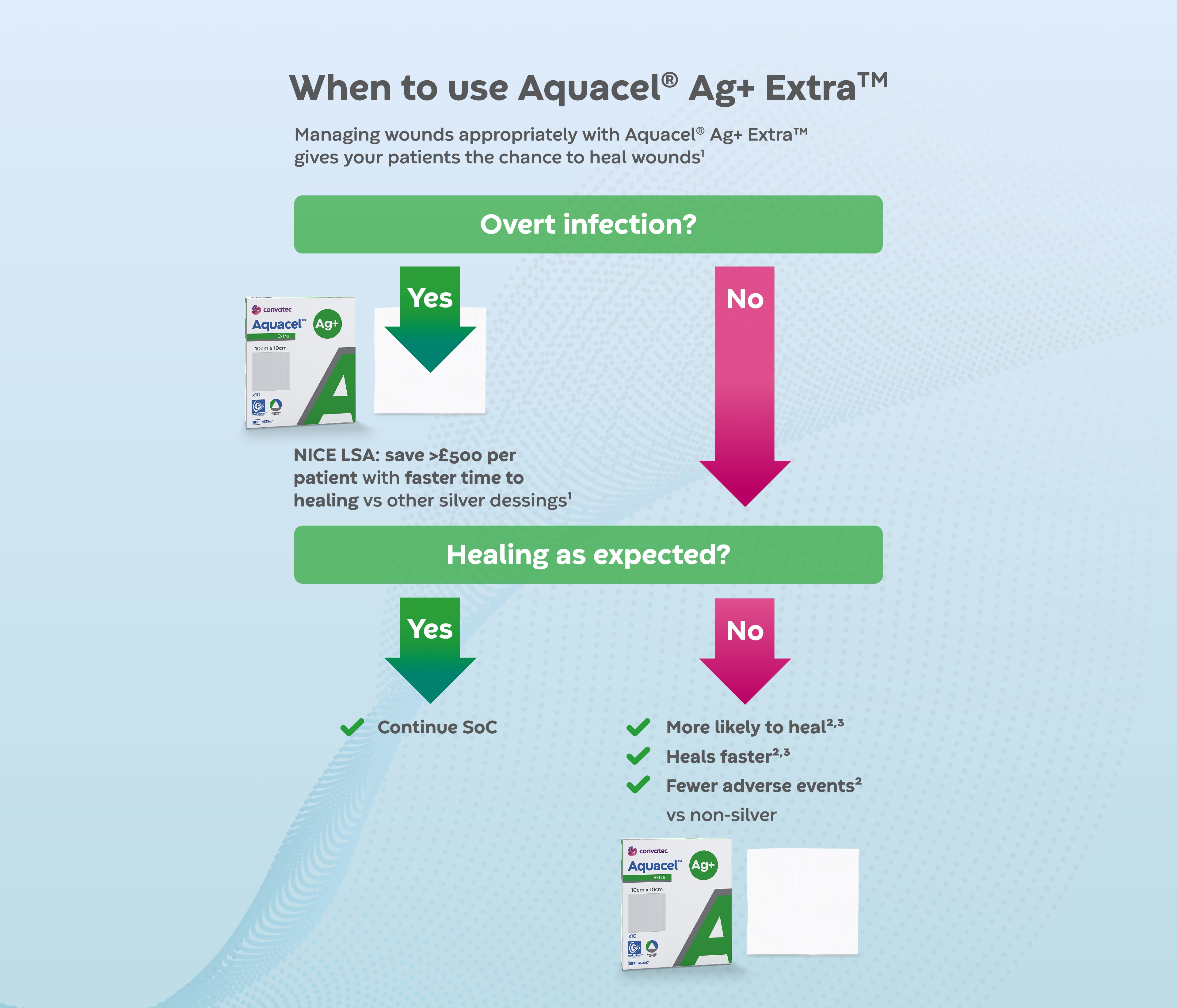
When to use Aquacel® Ag+ Extra™
The 3 components of Aquacel® Ag+ Extra™ with its More Than Silver™ technology, ensure that it’s specifically designed to address the issue of biofilm and contribute to wound healing.
- Chelating agent to disrupt, breaking down biofilm matrix⁹⁻¹¹
- Surfactant to weaken, loosen and remove biofilm allowing absorption by the dressing¹⁰⁻¹³
- 1.2% ionic silver, a broad spectrum antimicrobial
Aquacel® Ag+ Extra™ in action
Baseline: 14-year old static wound
- Venous insufficiency
- Maanged with cleansing, debriding and antimicrobial dressings
- Compression and superabsorbent cover dressing for exudate
Intervention: 6 weeks with Aquacel® Ag+ Extra™
- Exudate managed with Hydrofiber®, reduced peri-wound maceration
- Healthy granulation formed, epithelialisation started
- Static wound progressing to healing
When to choose Aquacel® Ag+ Extra™
Managing wounds appropriately with Aquacel® Ag+ Extra™ gives your patients the chance to heal wounds
Key Takeaways
Silver dressings are not all created equally. NICE's LSA affirms that targeted use of advanced antimicrobial dressings like Aquacel® Ag+ Extra™ is supported by robust evidence and can be a significant dressing in infection and biofilm management.
References
1. Holmes et al [GID-HTE10041] – Topical Antimicrobial Dressings for Infected Leg Ulcers in People 16 and over. Second Addendum; NICE, York Health Economic Consortium. 2025.
2. Holmes et al [GID-HTE10041] – Topical Antimicrobial Dressings for Infected Leg Ulcers in People 16 and over. External Assessment Group Report; NICE, York Health Economic Consortium. 2025.
3. International Wound Infection Institute (IWII) Wound Infection in Clinical Practice. Wounds International. 2022.
4. Stewart. Microbiol Spectr. 2015;3(3).
5. Malone et al, J Wound Care. 2017;26(1):20-25.
6. Murphy et al, J Wound Care. 2020;29(Suppl 3b):S1-28.
7. International Wound Infection Institute (IWII) Wound Infection in Clinical Practice. Wounds International, 2022.
8. Wolcott et al. J Wound Care. 2010;19(8):320-328.
9. Banin 2006, Chelator Induced Dispersal and Killing of Pseudomonas aeruginosa Cells in Biofilm
10. Parsons 2016, Enhanced Performance and Mode of Action of a Novel Antibiofilm Hydrofiber® Wound dressing
11. Said 2014. An in vitro test of the efficacy of an anti-biofilm wound dressing
12. Chen 2000, Biofilm removal caused by chemical treatments
13. Meredith 2023, Assessment of Silver-Containing Gelling Fiber Dressings Against Antibiotic-Resistant Pathogens Using an in vitro Biofilm Model
14. Beraldo S, Ljungqvist J, Rodger R, Hanson B, Saavedra C. Effectiveness of an enhanced silver-containing dressing in hard-to-heal venous leg ulcers: a randomised controlled trial. J Wound Care. 2025;34(3):170-178.
15. Meaume S, Truchetet F, Cambazard F, et al. A radomized controlled, double-blind prospective trial with a Lipido-Colloid Technology-Nano-OligoSaccharide Factor wound dressing in the local management of venous leg ulcers. Wound Repair and Regeneration. 2012;20(4):500-511. doi:10.1111/j.1524-475X.2012.00797.x
AP-76380-GBR-ENG-v1
Blogs